🔍 The Industry Problem, Challenges & Opportunities
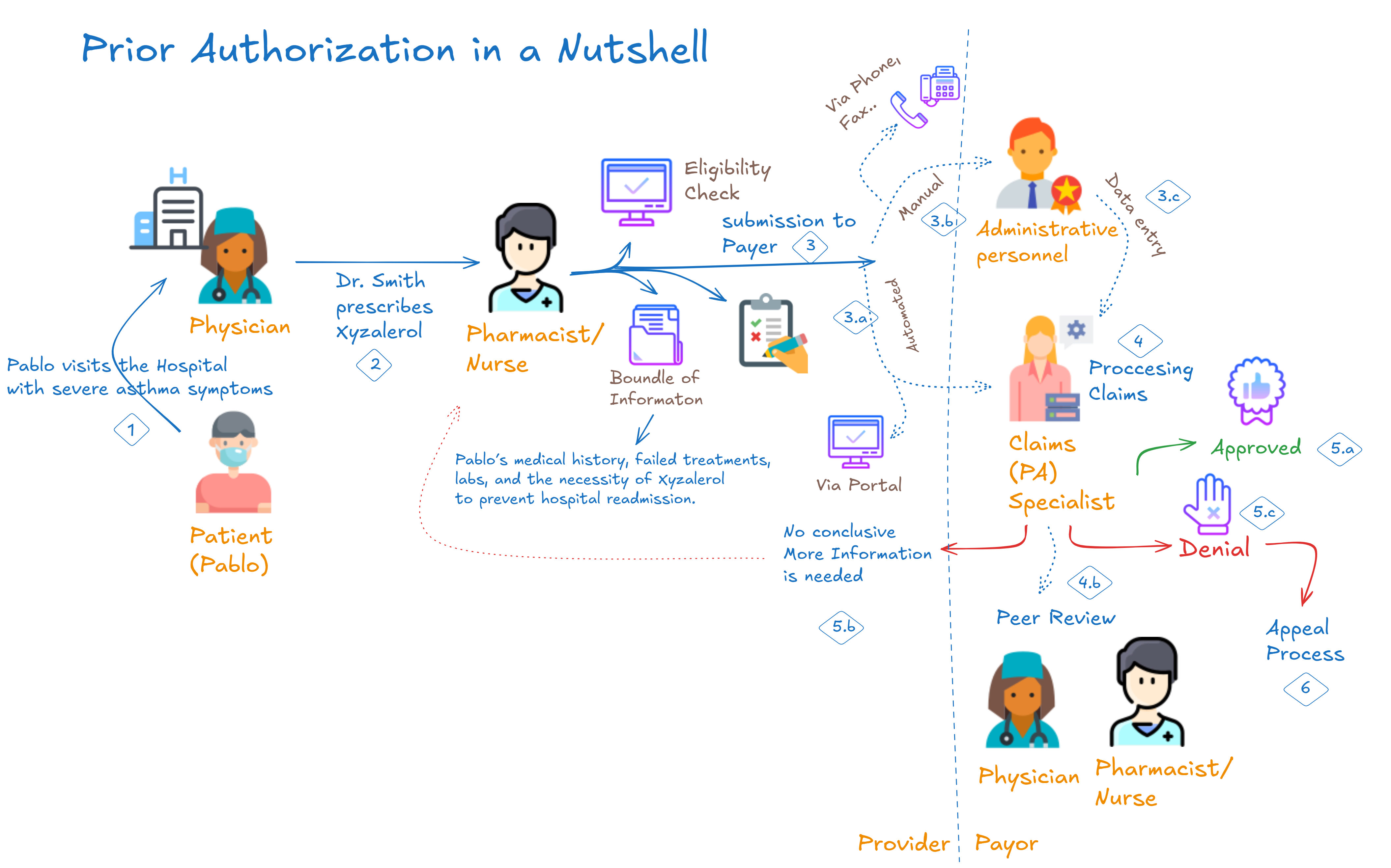
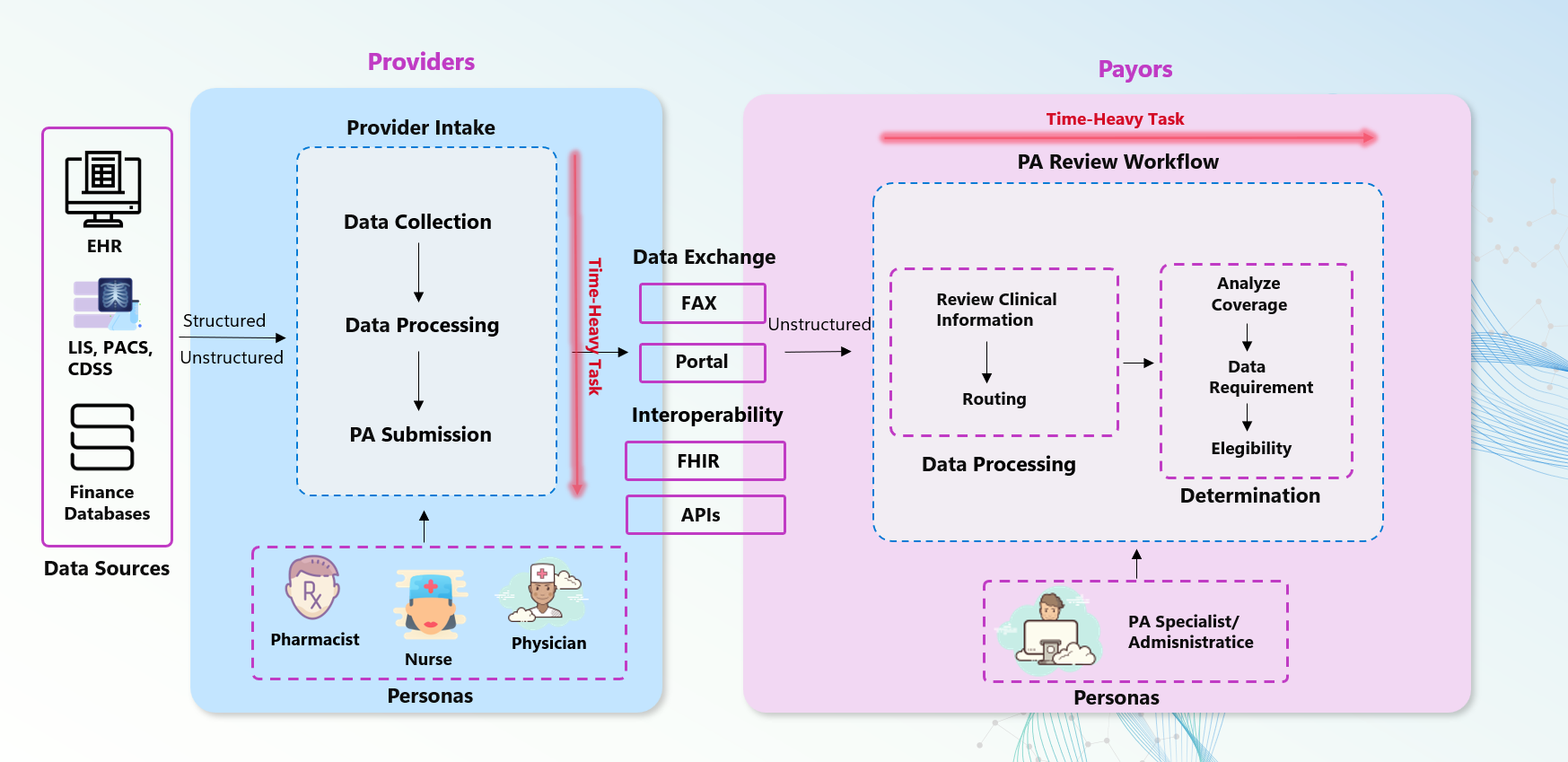
Prior Authorization (PA) serves as a critical checkpoint before delivering certain healthcare treatments. Despite its importance, today’s PA processes are plagued by delays, manual reviews, and costly inefficiencies.
Key Pain Points
Providers
- 41 Requests per Week: Physicians handle an average of 41 PA requests per week, consuming around 13 hours—equivalent to two business days.
- High Administrative Burden: 88% of physicians report a high or extremely high administrative burden due to PA processes.
- Treatment Delays: 93% of physicians report that PA delays access to necessary care, leading to treatment abandonment in 82% of cases.
- Mortality Risk: Even a one-week delay in critical treatments like cancer increases mortality risk by 1.2–3.2%.
Payors
- Manual Processing Costs: Up to 75% of PA tasks remain manual, costing around $3.14 per request.
- High-Volume Approvals: Payors face challenges in automating low-risk cases, often leading to bottlenecks in processing.
- Reduced Accuracy: Manual errors can result in up to 75% inaccuracies in approval decisions, increasing provider frustration and potential compliance risks.
Patients
- Negative Health Outcomes: Delayed care significantly affects patients, especially in critical care scenarios like oncology, where even slight delays worsen outcomes.
- Treatment Abandonment: Long wait times discourage patients, leading to dropped care and increased long-term healthcare costs.
Regulatory and Industry Trends
CMS 2026 Regulations
- Mandated Real-Time Data Exchange: Payors are required to use APIs based on HL7 FHIR standards to facilitate quicker PA decisions—72 hours for urgent cases and 7 days for standard requests.
- Transparency Requirements: Payors must now provide detailed explanations for PA decisions, fostering trust between providers and payors while ensuring compliance.
The Push for Automation
- Demand for AI Integration: Automation technologies like AI/ML are gaining momentum, promising to reduce manual efforts, improve approval accuracy, and cut costs significantly.
- FHIR-Driven Interoperability: Healthcare IT systems are rapidly adopting the FHIR standard, enabling seamless data sharing and decision-making.
Challenges Highlighted
- Operational Inefficiencies:
- Providers often lack real-time insight into PA requirements.
- Transparency issues result in delays and bottlenecks.
- Cost and Time Concerns:
- Payors spend up to $3.14 per manual transaction.
- AI-enabled systems can cut costs by 40%, reduce manual effort, and improve decision-making speeds from days to hours.
- Patient Risks:
- Delayed treatment exacerbates conditions, leading to poor health outcomes.
- Automation can enhance access and patient satisfaction by reducing turnaround time.
Automation and Opportunities
By leveraging AI-driven automation, PA processes can be streamlined with the following benefits:
- 40% Reduction in Processing Costs: AI-enabled auto-approval mechanisms drastically reduce costs in high-volume cases.
- Enhanced Provider-Payor Communication: Transparent, real-time decision-making builds trust and efficiency.
- Improved Patient Outcomes: Faster PA approvals ensure timely care delivery, reducing mortality risks and abandonment rates.